Is back pain, hip pain or leg pain affecting your quality of life? Don’t put up with it any longer.
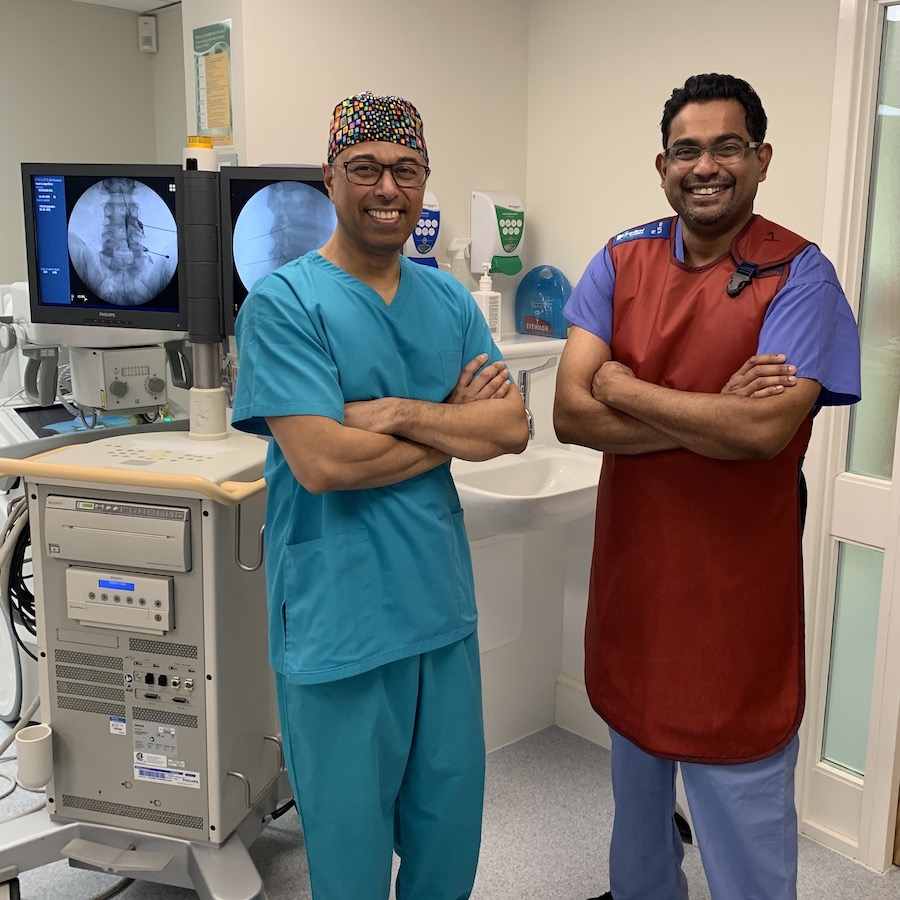
Professor Mushtaque Ishaque is one of the UK's leading orthopaedic specialists and he has helped thousands of patients from Birmingham and all over the world discover a new lease of life, free of pain and without undergoing surgery.

“Having suffered from severe back, leg and hip girdle pain myself, I know how it can affect a patient and their loved ones: how it can render you immobile for days on end, unable to do the things you once enjoyed without a second thought.
What most sufferers don’t realise that their back pain or leg pain is actually a spinal issue, so it can be misdiagnosed or not diagnosed at all - causing prolonged and unnecessary suffering for patients. My practice is dedicated to diagnosing the real source of your pain using the latest MRI imaging technology and then developing a treatment plan which is graduated and personalised to your individual needs, using conservative and minimally-invasive options (such as spinal injections) first.
My ethos is that surgery must always be the last resort. In fact, most patients don’t need surgery - even if they have already been told by other consultants that they do need surgery. I routinely offer my patients a minimally-invasive approach so that they experience the best possible outcomes with the least amount of disruption to their lives. I hope that I can help you too, just as I have helped thousands of others before you.”
Professor Mushtaque A. Ishaque
Consultant Spinal Surgeon
BSc(Hons) MB BChir(Cantab) DM FRCS FRCS(Ed) FRCS(Orth)
Our services and what we treat
Most of our patients come to us without having had a formal diagnosis as to what is causing their back pain or leg pain. They may have had some treatment attempted, but the real source of the pain is still unknown. Our job is to take control of the situation, quickly find the cause of the pain by utilising the latest MRI scanning technology and Professor Ishaque's decades of expertise, and then implement a full management plan to ease the pain.
We also welcome patients who are looking for a second opinion. Professor Ishaque frequently sees patients who have been told they need surgery, when in fact other non-invasive treatment may be more suitable.
The patient journey
We pride ourselves in offering a swift service where an initial consultation appointment can be made, diagnostic tests performed and a full diagnosis and personalised treatment plan created for you by Professor Ishaque - in just one week.

Introducing Ms Linda Hamilton
Linda has been Professor Ishaque's private secretary for many years, and is frequently praised by patients for her dedication to making the patient journey as smooth as possible for them. She will be your primary contact for any queries while you are under our care.

Initial consultation
At our clinic in Birmingham or even as a remote appointment, Professor Ishaque will listen carefully to you to understand your issues and may also conduct some basic tests during the initial 30 minute appointment. You’ll be able to ask any questions and voice any concerns you may have about your care in a safe, supportive environment.
Diagnostics
If Professor Ishaque deems it necessary, full diagnostic tests such as an MRI and a standing X-ray may be ordered so that he can make an informed diagnosis. These can take place with the results available just 3-4 days after the initial consultation.

Followup consultation and personalised treatment plan
A follow up appointment would have already been booked in anticipation of the test results being available. Professor Ishaque will discuss these with you, and put together a personalised treatment plan (such as spinal injections) to put you on the road to recovery with regular assessments of how your condition is improving.
Surgery (as a last resort)
If Professor Ishaque feels that surgery would be the best option for you, he will be able to refer you to a surgeon who performs that operation regularly to ensure that you have the best chance of the getting the best outcome.
Testimonials
Stuart Went
“I would like if possible to add a testimony for the superb treatment and care Professor Ishaque has provided.”
I have been suffering with lower back pain for a number of years which has lead to spasms and discomfort down my left leg when standing for periods of time and participating in various sports. Strength work , rest etc didn’t lead to any relief. Going through the diagnosis process with Professor Ishaque was super informative and eloquently explained what was going on.
Gwyn Bispham
“I would have no hesitation in recommending Professor Ishaque to anyone. A first class experience from beginning to end.”
Having suffered extreme back and leg pain for several months, I looked for a solution on the internet and discovered the brilliant Professor Ishaque. I found his excellent website comprehensive, full of information and advice. I was particularly struck by his caring approach to his patients, so didn’t hesitate to book an appointment. My first consultation was unexpectedly warm and welcoming. I quickly forgot my nerves and felt more at ease.
Contact us
If you’d like to make an appointment, please email [email protected] or telephone 0121 446 1674 to speak to a member of our team.